New stroke guidelines
Episode 13, 22 September 2017
The Stroke Foundation recently released its updated Clinical Guidelines for Stroke Management, to help health professionals to deliver the most up-to-date, evidence-based stroke treatment. But what do these guidelines say and what do they mean to stroke survivors and their carers?
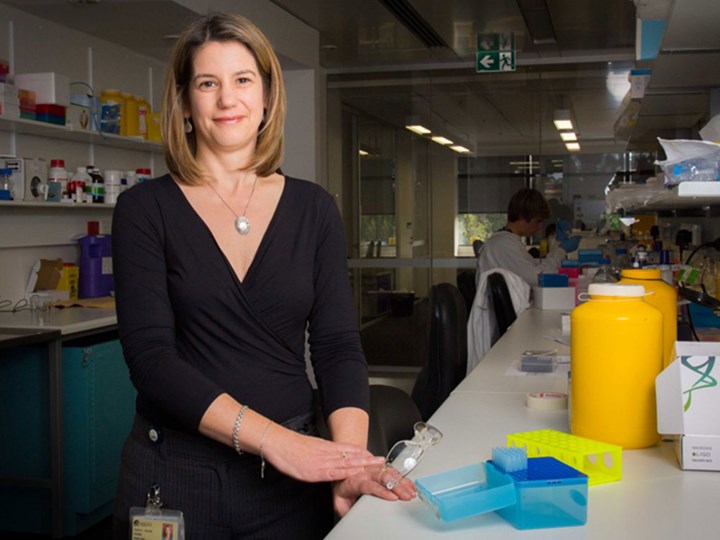
To find out, we talk to physiotherapist Assoc. Prof. Coralie English, a researcher from the University of Newcastle and the Hunter Medical Research Institute, and Co-chair of the Content Development Working Group for the Clinical Guidelines.
Podcast transcript
Announcer: Welcome to the EnableMe podcast series, where we bring together stroke survivors, health professionals and researchers providing you with practical advice. To enable you to on your journey to reclaim your life after stroke.
You can join the conversation at .
This series is presented by Australia's national Stroke Foundation.
Chris: The Stroke Foundation recently released its updated Clinical Guidelines for Stroke Management. These guidelines help health professionals to deliver the most up-to-date, evidence-based stroke treatment. But what do the guidelines say and what do they mean to stroke survivors and their carers?
Well to find out, I am talking to physiotherapist Dr Coralie English. Coralie is a researcher at the University of Newcastle and the Hunter Medical Research Institute, and she was Co-chair of the Content Development Working Group for the Clinical Guidelines. Thanks for speaking to us, Coralie.
Coralie: My pleasure. Thanks for the opportunity.
Chris: Now, I mentioned that you were the co-chair for the guidelines development. I should mention that was along with Associate Professor Bruce Campbell from the Royal Melbourne Hospital. Look, it sounds like a very important role, but what did it involve from your point of view?
Coralie: The role was one of overseeing the content development of the guidelines. So the project of rewriting the guidelines was a massive one as you can appreciate, and was supported by a team of people at the Stroke Foundation from the project perspective, and also a huge number of people from around Australia from the clinical perspective.
The role that Bruce and I took on as co-chairs of the content development, was to ensure that the processes were followed and to gather and lead groups of people around Australia who helped to review the evidence, pull out the data about what evidence we had for particular clinical questions and to, on that basis, write our particular guideline.
And this year our ... or this update of the guideline is far more detailed than our previous ones, in that we have readily available all the details of the evidence underpinning each recommendation, but also probably more importantly, easy to read summaries of that information and practical guidance about how best to implement them in the clinical setting.
So Bruce and my role was to oversee all of that, across all the different questions and different parts of the guidelines from pre-hospital care all the way through to secondary stroke prevention and living with the effects of stroke. So our role was to oversee all of those and ensure that the processes were followed and that the content was appropriate and easy to digest.
Chris: Okay. Now you mentioned going through various questions and all the evidence involved so, I understand that it is really a matter of taking the research evidence and turning it into recommendations for health professionals. How does that process actually work though?
Coralie: So it's a very involved process, as you can appreciate. It starts with very comprehensive searching of all the published evidence that we have for stroke around the world, and that in this update really took us by surprise, just how much more evidence in the various aspects of stroke care had been published in the seven years prior to the 2010 guidelines. There's been a huge increase in the research available.
The first step is to find all of that research. Prior to that actually, the first step is to define all the different particular questions we want to know, in terms of all the different aspects of stroke care, and then to do specific searches for evidence for what we know about what the effective interventions are for each of those clinical questions.
Then it's a process of deciding what the best level of evidence is, what's the most believable piece of evidence in there, and then understanding what that means for clinical practice and how that evidence could be applied to people after stroke.
Chris: Okay so what are some of the highlights that have come out of the guidelines then, from your point of view?
Coralie: So I had the responsibility of overseeing the rehabilitation side of the guidelines, so that's the bit that I can speak to more authoritatively, but some key highlights were that there was a very, very large rehabilitation trial known as AVERT, A Very Early Rehabilitation Trial, which helped us to understand what people should be doing early after stroke in terms of getting out of bed and getting moving.
That one was particularly challenging to write, because the outcome of that trial was unexpected in that overall the outcome was if you get people up too early and work them too hard it can actually be harmful. So we have some recommendations about not starting rehabilitation too soon, as in less than 24 hours after stroke, but it also gave us some good guidance that for most people, getting up frequently for short bursts of activity after at least 24 hours after stroke is really beneficial.
The other key highlight for me is understanding that more rehabilitation is probably better for people after stroke later, so we're now talking in the days and weeks after stroke. So we now have stronger guidelines and better numbers to pin that on so we can guide health professionals as to how much therapy they should be providing for their people after stroke.
In the early stages, from the acute care perspective, the outcome of some really exciting trials in clot retrieval, so that basically means interventions that go into the brain and pull out blood clots if you had that type of stroke. We now have good evidence that that procedure is really effective, so we have some guidelines around the implementation of that as well, which is a real game changer and can be a lifesaving treatment for people after stroke.
Chris: Okay, I understand that a lot of that work on that clot retrieval like you mentioned, that was done here in Australia. I think your colleague Bruce Campbell was involved in some of that research, is that correct?
Coralie: Yes, that's right, yes. And that's really the face of stroke trials both in the early stages and in rehabilitation. We’re really moving towards research that's been done on the international stage, so there's a lot more collaboration and team work to answer these really big questions that often can't be answered in one trial alone or at one centre.
So there's a lot more trials that are now national and international that Australian researchers are part of, but we're also very much world leaders in setting up these trials and running them and getting our partners internationally to be involved as well.
Chris: Now you are a researcher yourself, can you just give us an idea of what things you look at, and how that fits into the sort of stuff that's covered in the guidelines?
Coralie: My particular interest is in physical activity and also how much practice and how much rehabilitation people get after stroke.
So my early PhD and early post-doc work focused on the use of circuit class therapy in stroke rehabilitation. So essentially that means the idea of, for people receiving physiotherapy services after stroke who need to improve their walking, that rather than having just one appointment with a physio each day in rehab, that instead they spend longer time in group settings to enable more practice of the things that they need to do to get better.
So those studies are directly referenced in the guidelines and are part of the recommendation about providing as much therapy as possible to people after stroke, when they're at inpatient rehabilitation facilities.
The other work that I've branched out into since then, and has been supported by various Stroke Foundation research funding through the years as well, is focusing on the impact of exercise for people after stroke and how that can help in secondary prevention, and also the effects of sitting down for too long every day that we all know is bad for our health. And there's potential benefits for people after stroke if they can't get up and exercise at a really intensive level, about whether they might be able to just reduce some of their sitting time each day and replace that with a little bit of lighter intensity activity.
So that's the sort of work I'm focusing on at the moment, and really it can be summed up in terms of how much and what type of exercise people need to do after stroke, and are there benefits of doing a little bit. We tend to focus on the big guidelines that you should be doing 30 minutes of exercise most days of the week, which is really hard for most of us and even harder of course for people after stroke.
So I'm really interested to know, whether little amounts of exercise and perhaps little amounts of less intense exercise, may be important for people to reduce their stroke risk and secondary stroke risk, and might be more achievable for them as well.
Chris: Well it's great to hear that research like that is, I guess, still going and that we're constantly going to be seeing new improvements in stroke treatment. With the current guidelines though, do you think that will lead to some big improvements, or big changes to people?
Coralie: Yes absolutely. And I think that the next challenge… So while this was a massive project and two years of work with countless hours of, voluntary hours from people all around Australia who contributed to the guidelines, it's really just the first step.
And the next big push is to how we can implement these guidelines in a clinical setting, what practice changes need to happen so that the implementation is optimal, and that is no mean feat at all.
The other thing that's really important to mention, that we really need to be pushing for, is to be able to move to something called “living guidelines”.
So it was seven years between the previous Stroke Foundation Clinical Guidelines and these updates, and it was you know a huge job to do that. The way that we've done it this time in using the MAGICapp platform and having them online, gives us a functionality to move towards what's called living guidelines, so that we can update our recommendations as new evidence comes out, which is happening at a faster and faster rate.
But to do that we need support and funding for the Stroke Foundation to move towards that. So I think that's a really important thing that we should all be aware of and look for opportunities for, because that's really going to be the thing that makes the biggest difference in making sure everybody who has a stroke has the best possible care based on the best up-to-date evidence at any point in time.
Chris: I guess it's a good message, I suppose, as you said, support the Stroke Foundation, but also people are aware of this and that the importance say for their politicians to back, maybe fund some of these guidelines as well.
Is there other things that people should be doing, I suppose, in response to the guidelines? I mean, it is something clearly that we want the health professionals out there to pick them up and to adopt them, but what about people like stroke survivors and carers, is it worth them being across what the guidelines recommend, or is it just a matter of making sure that they have health professionals who do follow them?
Coralie: Look, I think both is really important. I think the guidelines in the format that they're written have been directed at health professionals. They're about what we're trying to inform people as the best evidence of what sort of treatments and interventions they should be providing for their clients and the people that they're seeing who've had a stroke.
But we had a consumer representative as part of the guideline development, which was really, really important, and that needs to continue, that input of are we asking the right questions of the evidence? Is there things ... we couldn't include everything we wanted to in these guidelines. As it is we have 250 recommendations. So there were some things that we couldn't specifically include that if we can move to living guidelines we'd be able to add to.
So it's important for the stroke survivor community to let us know if there's guidelines that are missing, that they want to know the evidence for particular things, but also that they're… because the guidelines are online and they're freely available, of course we encourage people who've had a stroke and their family and carers to have a look at the relevant sections for them, and to then be able to have that discussion with the health professionals working with them about what the guidelines say and what interventions and treatments they're receiving, to become informed consumers of healthcare as well. And that I think will help to drive the implementation of these guidelines into best practice.
Chris: Fantastic. Well that is, I guess, a good message and something of course that we will support. We will be putting the links to more information on the Clinical Guidelines up on enableme.org.au, and of course encouraging health professionals to access the full information, including all the research, at our website informme.org.au.
Thank you once again for talking to us, Coralie, and look, it is a massive job and I think you've done excellent work there.
Coralie: Thank you very much. It was great talking with you.
Chris: Fantastic. That was physiotherapist and guidelines co-chair Dr Coralie English.
Just remember that stroke survivors and carers, if they want to find out about any other topic they can also call StrokeLine on 1800 787 653 or 1800 STROKE, or they can ask a question through EnableMe and get a response from health professionals and other stroke survivors.
And that is it for our podcast today, if you like what you've heard please give us a good rating and review on iTunes so that you can help other people to find our podcast.
Thank you once again to our guest Dr Coralie English.
Announcer: That's all for today's EnableMe podcast. You can find out more on this topic and continue the conversation or listen to other podcasts in the series at our website enableme.org.au.
It's free to sign up and you can talk with thousands of other stroke survivors, carers and supporters. We also have health professionals from StrokeLine who can answer your questions and give evidence-based advice.
The advice given here is general in nature and you should discuss your own personal needs and circumstances with your health professional. If you would like to suggest a topic or provide feedback, contact us via the website enableme.org.au.
Announcer: The music in this podcast is “Signs” by stroke survivor Antonio Iannella and his band the Lion Tamers. It was recorded at Antonio's studio, which you can find out more about at www.studiofour99.org.au.
This EnableMe podcast series is produced by the national Stroke Foundation in Australia.

